What was claimed
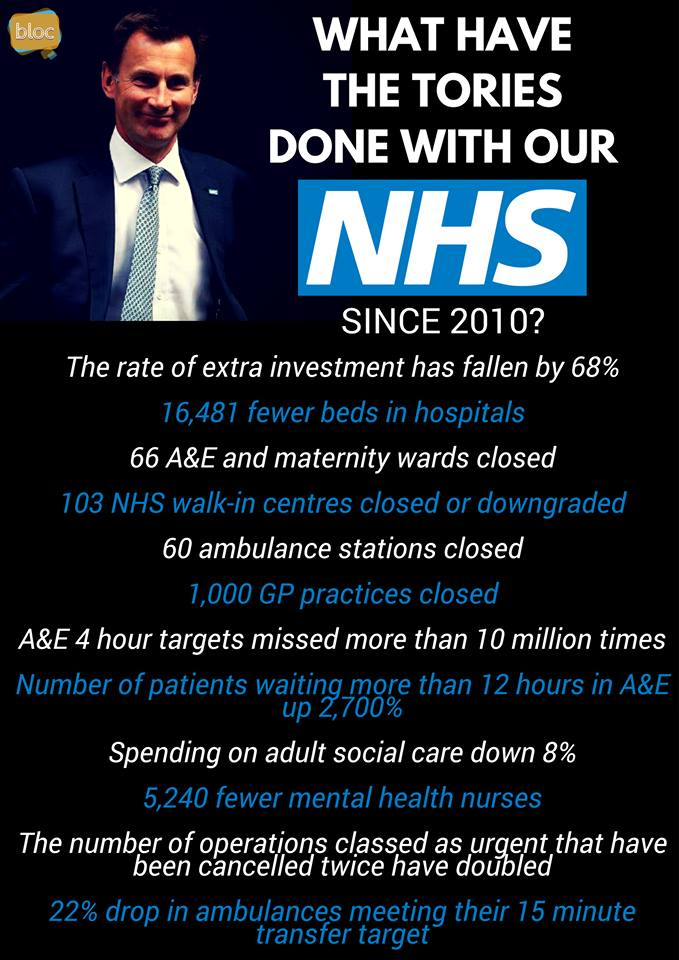
The rate of extra investment in the NHS has fallen by 68% since 2010.
Our verdict
Correct, although this refers to growth in all UK health spending, rather than just for the NHS. It compares the periods 1955/56 to 2015/16 (when health spending grew by an average of 4% in real terms each year) and 2009/10 to 2015/16 (when it grew by an average of 1.3% a year).